
HSC Transformation
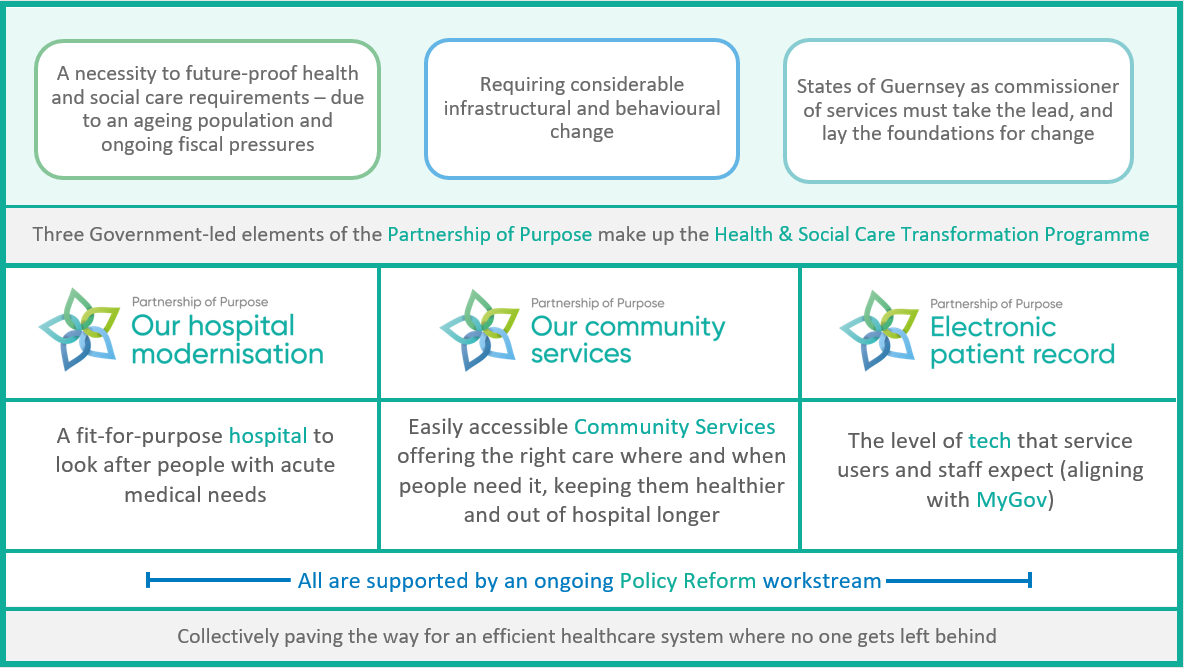
The Partnership of Purpose represents a major overhaul of how islanders will look after their health and wellbeing and access the care they need going forward. It was instigated by a 2017 Policy Letter to the States of Deliberation which recognised that our current health and social care model will not cope with future demand, largely due to our ageing population.
In many cases, services need to be brought up to acceptable modern standards, with the essential upgrades to the Princess Elizabeth Hospital perhaps being the most obvious. But our health and social care services extend so far beyond the hospital, and the overall objective of the whole system is to keep people as healthy as possible and out of hospital. This means that ensuring all the non-acute community-based health and social care services are equally fit-for-purpose and easy to find is just as important.
So simply put, The Partnership of Purpose is about making our health and social care provision as efficient as possible. It's about empowering people to lead healthier and happier lives while knowing how to access to the right care when they need it.
It's a collective effort, calling on the public, private and third sectors, to work collaboratively to future-proof health and social care services. The States of Guernsey is taking the lead in facilitating this change.
A community-wide effort
Life expectancy is going up, which means if people keep accessing healthcare in the same way they'll need more of it throughout their lives and the system won't be able to cope with demand.
So the whole way we access health and social care needs to change. On the one hand, the services that the public, private and third sectors offer need to adapt. But equally importantly, individuals need to be encouraged and supported to be more proactive in leading healthier lives.
What do we mean by this? Think of it in the sense that some elements of our health are within our control - perhaps our general fitness or nutrition - whereas unfortunately some elements of our health are outside our control - like the risk of unexpected illnesses or aspects of our menial health. We should all be responsible for keeping as healthy as possible, in terms of what is in our control, as this will help free up health and social services for where they are needed the most.
An efficient healthcare system means people should always have access to the right care they need. If you need acute care there will be a hospital bed for you. If you need a GP appointment you should be able to book one promptly at a time that suits you. But it is in all our best interests to ensure we only call on these services when we genuinely need them. Adopting the right personal behaviours around health and wellbeing is key.
A preventative mindset is a bit of a buzz phrase, but what does that mean?
In one sense this might mean acting on any ailments swiftly. Prompt diagnosis will often lead to quicker and simpler treatment or cure. Better for the individual and less impact on the system.
A preventative mindset also means avoiding the risk of health complications in the first place, perhaps though better diet, exercise and general wellbeing. Some people will need a little helping hand to make those lifestyle choices. That might come from knowing the right charity to call on or self help route to go down, rather than a GP always being the first port of call. Every little behavioural change like this will help make health and social care provision more efficient. It's all about ensuring resources are targeted in the right way.
Progress
Over the last four years, HSC has been working with public, private and third sector providers to develop this new model of health and social care, with two key strands of work taking place to date:
1. Laying the foundations for the transformation, which has included:
- Progressing the design work to modernise the hospital site
- Exploring the development of complementary community hubs
- Procuring the new electronic patient record (My eHealth record) system
- Reforming how health and care funding is managed within the States of Guernsey
- Receiving approval for the future model of health and care regulation
2. Developing new and improving existed services aligned to the values of the Partnership of Purpose.
These have been wide ranging but have included the development of social prescribing, the commencement of a programme of joint strategic needs assessments to better inform how and where services are most appropriately provided and numerous projects looking to improve islanders' experiences, for example the introduction of a new diagnostic service in cardiology, advances in pain management and work to provide greater support to some local families.

HSC is now in a position where it can start formally accrediting those public, private and third sector partners working to realise the Partnership's values. As an initial step, the first five members of the Partnership of Purpose have been announced. Each organisation plays a different role in the overall Partnership; either by providing frontline healthcare services, raising awareness, seeking to shape future policy or providing preventative services to the community. Together they have demonstrated their commitment to working towards a healthier and happier Bailiwick.
Members of the Partnership of Purpose
Established in 2018 and bringing together public, private and third sectors, the Health Improvement Commission seeks to empower, enable and encourage healthy living in Guernsey and Alderney. Their work focuses on four main areas; Be Active, Eat Well, Healthier Weight and Substance Use. The importance of their role was clearly demonstrated throughout lock down as they supported islanders in eating well, through, for example, supplementing nearly 1000 Guernsey Welfare Service Food Bank parcels with approximately 8,630 adult portions of fresh vegetables and fruit and encouraging islanders to be active. They maintained access to weight management services through phone and online-based provision and the Substance Use work stream continued to offer information and practical help through the drug and alcohol agencies it supports. During those difficult times of lock down, it was vitally important to continue to provide local, confidential support for alcohol, drugs, domestic abuse and mental health. As our community moves forward, the Commission continues to advocate for environments which make it possible and easy to live healthily across the Bailiwick.
The local charity works to empower individuals to make positive choices about their reproductive and sexual health, providing an accessible, confidential and affordable service which provides non-judgemental, individualised advice. They work closely with a range of stakeholders to reduce the rates of unplanned pregnancies and abortions and are the main providers in the Bailiwick for free contraception for under 21s, a project jointly delivered with the States of Guernsey and which has seen teenage pregnancies reduce dramatically since it was introduced.
As the Island's only community based sports and leisure centre, and with a footfall of approximately 600,000 per annum, Beau Sejour plays an invaluable role in supporting islanders' access to physical activity. It is the only facility on-Island offering Exercise on Referral 'LifeFit' sessions (689 individual referrals made in 2019) and Aqua Health Referral sessions to the local community. In addition, the Active Health team deliver other specialist classes such as CanMove (exercise classes for individuals who live with or are recovering from cancer treatment) and MoveSmart (exercise classes for individuals with Multiple Sclerosis).
Working with HSC and the private sector, QRMP has developed the first genomic screening programme in the Bailiwick to identify and treat people with the genetic condition Familial Hypercholesterolaemia. The disease, which results in high levels of cholesterol that can lead to cardiovascular disease, the leading cause of preventable death in the developed world, is significantly under-diagnosed in the British Isles and the programme is aiming to be one of the most effective in the world.
While brought to prominence through COVID-19, Public Health provides a vital role ensuring our population is as healthy as possible. By assessing, measuring and describing health and wellbeing, as well as health risks, health needs and health outcomes for our population, Public Health Services provides the evidence for shaping health and care across the Bailiwick.
